Abstract
Purpose: To describe the clinical presentation, management approach, and outcomes of patients with Blue Rubber Bleb Nevus Syndrome
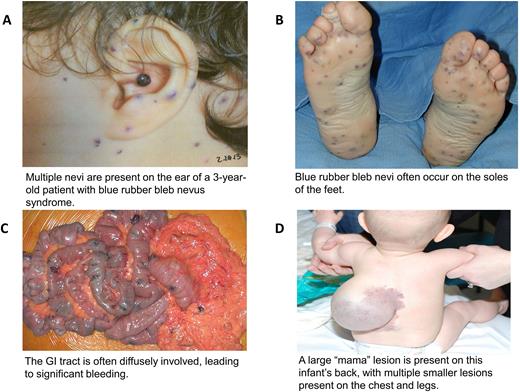
Background: Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare, congenital vascular malformation syndrome characterized by multifocal venous malformations involving the skin, gastrointestinal (GI) tract, and/or soft tissues. Severe iron deficiency anemia from GI bleeding is a frequent complication and patients experience significant transfusion burden. Iron supplementation and packed red blood cell transfusions are mainstays of supportive care in BRBNS. Although surgical resection, sclerotherapy, and medical therapy have been used to treat this disorder, prior data on the relative use of these treatment modalities and clinical response has been limited to single case reports or small (10 patients or fewer) case series.
Methods: A single-institution, retrospective review of 55 patients diagnosed with BRBNS was conducted. Data regarding demographics, clinical presentation, treatment, and response were collected.
Results: A total of 55 patients presenting to our Vascular Anomalies Center between 1993 and 2020 were evaluated. Overall, 91% of patients presented with a skin or soft tissue lesion, while 9% presented with anemia or GI bleeding. Patients were referred to our center by pediatricians (34%), gastroenterologists (19%), dermatologists (19%), or surgeons (19%). The median patient age at BRBNS diagnosis was 5 years (range: birth - 22 years). Most cases involved lesions of the skin (93%), GI tract (87%), or soft tissue (75%). GI involvement included the colon (75%), stomach (69%), small bowel (56%), duodenum (48%), esophagus (21%), and rectum (17%). Microcytic anemia (Hb < 2.5th percentile for age and MCV <2.5th percentile for age) was present in 82% of patients, with a median nadir hemoglobin concentration of 5.9 g/dL (range: 2 - 12 g/dL). Of the 55 total patients, 43 (78%) of all patients required packed red blood cell transfusions, with an average number of 31 transfusions per patient. Patients underwent sclerotherapy (91%), surgical resection of skin or soft tissue lesions (84%), surgical resection of GI lesions (58%), or endoscopic (cautery, band ligation) treatment of GI lesions (26%). After resection of GI lesions, 84% of had complete resolution of their symptoms. Fifteen patients (27%) received medical therapy with sirolimus, an mTOR inhibitor; 80% of those patients demonstrated response defined by improvement in anemia, improvement in GI bleeding, and/or diminished pain. Ninety percent of patients received more than one type of therapy. The median follow-up period for the cohort was 7.8 years.
Conclusion: BRBNS patients have widespread distribution of their lesions, including diffuse involvement of the GI tract. Many patients experience severe and often life-threatening anemia, often requiring significant transfusion support. A combination of surgical, medical, and interventional approaches is effective in treating BRNBS. In some cases, patients had complete resolution of their symptoms after surgical resection or medical therapy. Given the need for specific treatment, increased recognition of BRBNS by hematologists and referral to a center with expertise in vascular anomalies is important for optimizing outcomes for patients with this rare disorder.
Disclosures
No relevant conflicts of interest to declare.
OffLabel Disclosure:
Sirolimus is currently widely used for the treatment of vascular anomalies, but it is not FDA-approved for this indication.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal